Why Trauma-Informed Care Matters in Community-Based Brain Injury Services.
For individuals living with an acquired brain injury (ABI), recovery does not happen in a vacuum, and it rarely begins or ends with medical treatment alone. Long after hospital stays, rehabilitation units, and therapy appointments conclude, survivors and their families must navigate daily life in the community while managing cognitive, emotional, behavioral, and physical changes that can be both overwhelming and invisible.
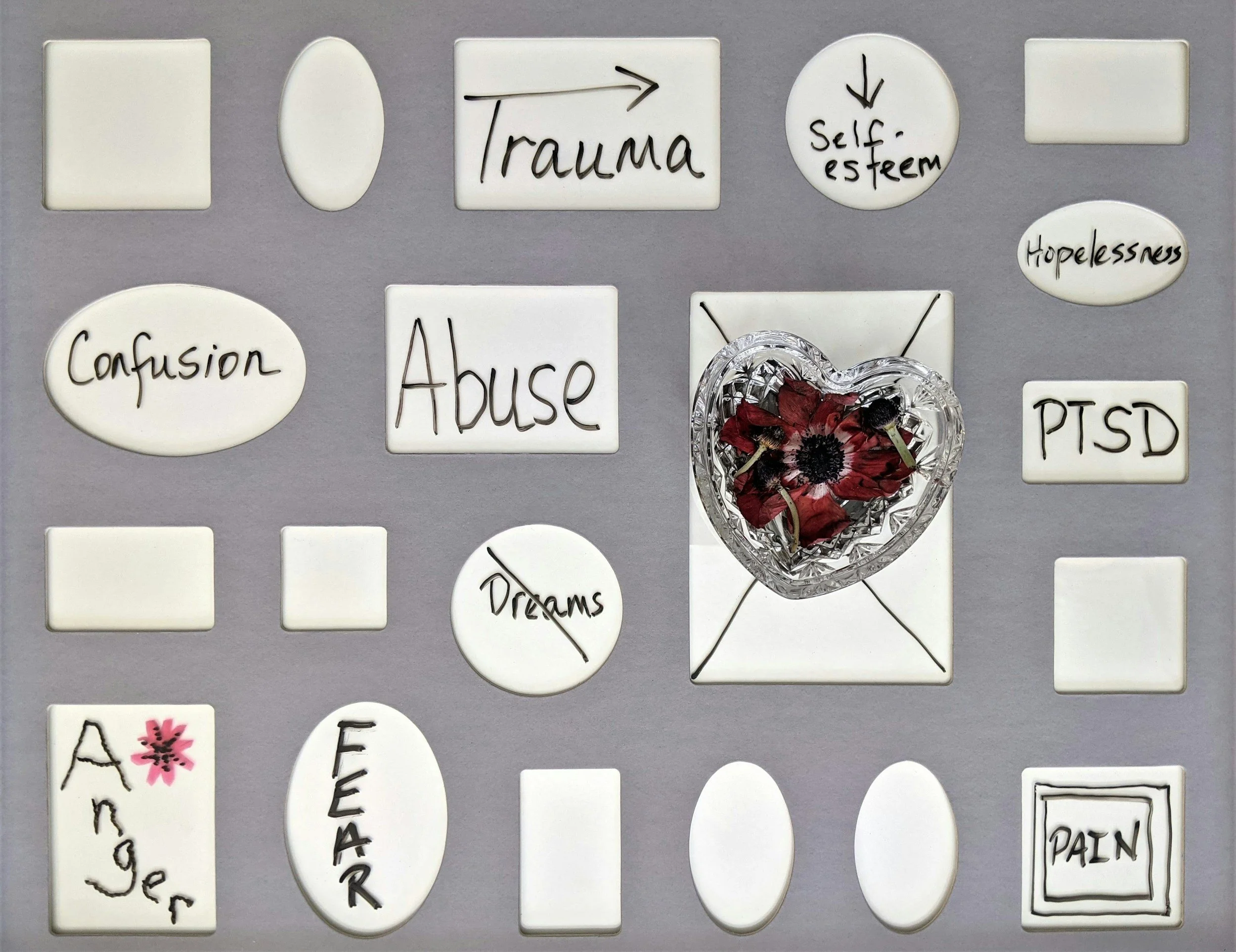
What is often overlooked in non-medical, community-based brain injury services is this critical truth: brain injury is almost always accompanied by trauma. When services fail to account for that reality, even well-intentioned supports can unintentionally cause harm.
This is why trauma-informed care is not optional in community-based brain injury services, it is essential.
Brain Injury and Trauma Are Inseparable
Trauma in the context of ABI can take many forms:
The injury itself (accidents, assaults, medical events)
Loss of identity, independence, or role within family and community
Repeated experiences of failure, misunderstanding, or exclusion
Systems involvement that prioritizes compliance over dignity
For many survivors, trauma is ongoing, not historical. Community-based services that ignore this reality may misinterpret trauma responses as “noncompliance,” “behavior problems,” or “lack of motivation,” leading to inappropriate interventions and reduced supports.
What Is Trauma-Informed Care in Community-Based ABI Services?
Trauma-informed care is not a single intervention or training; it is a framework that shapes how services are designed, delivered, and evaluated.
In non-medical ABI services, trauma-informed care means:
Understanding how trauma impacts cognition, emotional regulation, behavior, and trust
Prioritizing psychological safety alongside physical safety
Recognizing that resistance often reflects fear, overwhelm, or past harm, not unwillingness
Adapting expectations and environments to reduce re-traumatization
Building services with survivors, not for them
Most importantly, it means acknowledging that support must be flexible, relational, and person-centered, not system-driven.
Why This Matters in Non-Medical, Community-Based Services
Community-based providers are often present in the most vulnerable moments of a survivor’s daily life, at home, in the community, during transitions, and under stress. Without trauma-informed practice, services can:
Escalate behaviors rather than reduce them
Increase anxiety, shutdown, or avoidance
Undermine trust and engagement
Lead to unnecessary service reductions or placement changes
When trauma-informed care is present, survivors are more likely to:
Engage meaningfully in services
Build emotional regulation and frustration tolerance
Develop sustainable independence
Experience dignity, autonomy, and stability
Questions Survivors and Families Should Ask Before Choosing a Provider
Selecting a community-based brain injury provider is a major decision. Survivors and families should feel empowered to ask direct questions—and expect clear answers.
Here are critical questions to ask:
1. How does your agency define trauma-informed care in practice, not just in theory?
Listen for concrete examples, not buzzwords.
2. How are staff trained to recognize trauma responses versus “behavior problems”?
Providers should be able to explain how cognition, trauma, and emotional regulation intersect after brain injury.
3. How do you adapt services when a client is overwhelmed or struggling?
Rigid service models are a red flag.
4. How is person-centered planning actually implemented?
Ask how often plans are reviewed, who is involved, and how client voice is honored.
5. What role does consistency and relationship-building play in your services?
High staff turnover or task-based models can be destabilizing for trauma survivors.
6. How do you support autonomy and choice while maintaining safety?
True trauma-informed care balances structure with respect for independence.
7. How do you collaborate with families, therapists, and other providers?
Trauma-informed systems do not operate in silos.
Red Flags to Watch For
Families and survivors should be cautious of providers that:
Use compliance-based language (“won’t,” “refuses,” “noncompliant”)
Reduce services as a response to behavioral escalation
Cannot explain how trauma informs their approach
Rely heavily on one-size-fits-all programming
Prioritize cost or convenience over individualized support
Trauma-Informed Care Is About Respect, Not Control
At its core, trauma-informed care in community-based brain injury services is about recognizing the humanity of the person behind the diagnosis. It asks providers to slow down, listen more closely, and design supports that acknowledge the full lived experience of brain injury, not just what is written in a care plan.
Survivors deserve services that promote healing, safety, and dignity, not systems that inadvertently recreate harm.
Choosing the right provider can make the difference between merely surviving in the community and truly living within it.